 S2K Commerce - Products Dropdown
S2K Commerce - Products Dropdown
 Web Content Viewer - Blog
Web Content Viewer - Blog
The Comprehensive Dental Unit Waterline Testing Guide

What is in your dental unit waterlines?
You’ve probably seen the pictures and you’ve probably read the news headlines - looking for the answer to this question is not without stress.


While dental waterline contamination has gotten more attention the last couple years, this is a danger that the dental industry has struggled to understand or control.
In fact, at the Organization for Safety, Asepsis, and Prevention's (OSAP) Annual Conference last year, infection control experts Shannon Mills and John A. Molinari were asked the question, "What is the most pressing challenge in infection control facing dental professionals over the next five years?" they both responded without hesitating, "Dental unit waterlines".
The tough part about maintaining dental waterlines - and infection control, in general - is that dental professionals are not and should not be experts in waterline science. We, your patients, sit in your chairs every few months trusting you to be fantastically educated and skilled medical professionals, not water scientists.
But nonetheless, dental waterline safety best practices need to be understood and followed in every practice so that your patients are safe during procedures.
One of those best practices is regular dental waterline testing.
WHY TEST YOUR DENTAL UNIT WATERLINES?

Because on average even treated waterlines fail testing nearly 1/3 of the time. And non-treated lines are likely to have counts 200 to 400 times the CDC guidelines of ≤ 500 CFU/mL.
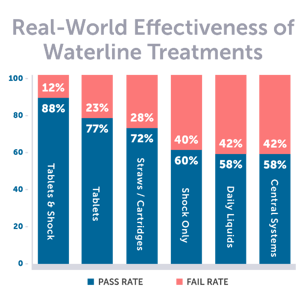
ProEdge completed a study of over 22,000 consecutive waterline tests from our water test clients measuring the effectiveness of all major products in real-world settings. Cited in a peer-reviewed article by John A. Molinari, PhD and Nancy Dewhirst, RDH, BS, this study revealed that 30% of treated lines fail to meet the ≤ 500 CFU/mL standard and some products performed significantly worse.
While using a high-level disinfectant to "shock" your waterlines and adding a low-level antimicrobial treatment to continually maintain them are both necessary for every effective treatment protocol, no treatment product is perfect, instructions for use (IFUs) can be difficult to follow, and biofilm never quits entering the lines to multiply and spread.
This is why testing your dental unit waterlines regularly is not only necessary, but recommended by the CDC, ADA, and OSAP, as the only way to ensure your dental water is safe.
"Every dental facility is responsible for meeting the minimum DUWL standards to ensure patient and dental-worker safety. Testing waterlines is the most reliable way to confirm and document that dental-water quality is acceptable." - Nancy Dewhirst, RDH, BS
WHAT KIND OF DENTAL WATERLINE TESTS ARE AVAILABLE?
There are two basic types of dental waterline tests: mail-in water test services and in-office waterline tests. Each have their advantages and disadvantages.
IN-OFFICE WATERLINE TESTS
In-office waterline tests are designed to be more economical and timesaving. These simple tests enable a dental professional to test their waterlines without leaving the office. Each test requires a sample taken directly from each unit and left to incubate for 2-5 days depending on the method they use.
In-office water tests are great for giving a practice a "baseline" for the current safety status of each waterline.
If used more frequently, in-office waterline tests "may help ensure staff compliance" and can provide early warnings of problems with your protocol (OSAP).
While these tests are found to be less reliable than laboratory testing, their purpose isn't to get the most accurate microbial count - that's the purpose of laboratory testing. Instead, these quick tests provide actionable results based on more of a pass/fail baseline so your office can take fast action if biofilm starts to gain ground.
THE ONLY IN-OFFICE WATER TEST DESIGNED FOR DENTISTRY


Order Today!
Make sure the in-office test you use includes germicidal neutralization for more reliable results. Not only is it recommended by OSAP, but neutralization is really important for accurate results.
Pay close attention to the IFUs as some bacteria can present in ways that are difficult to read. Dental professionals will also be required to keep their own records in case of inspection.
Should a complaint or infection lead to an office inspection, it is best to have validated laboratory testing reports showing safe water. For this reason, in-office waterline tests are recommended to be used in conjunction with laboratory testing.
MAIL-IN LABORATORY TESTING
Mail-in dental waterline testing kits from laboratories can often be purchased through your product supply company. Labs like ProEdge will send you a complete waterline kit with everything necessary to take samples, keep them viable, and return ship to the lab overnight. Samples incubate for 7 days and a test report with your results is emailed to your team.
Usually, laboratory testing uses advanced technology, trained specialists, and scientific methods to ensure accurate results. They also provide independent reports that can assist an office if inspected by regulatory agencies or if patients ever ask questions.
WHAT TESTING METHODS ARE MOST RELIABLE FOR A DENTAL PRACTICE?
The methods available to dental professionals for testing their waterlines have similarities and differences. First, we'll look at the similarities.
All current dental waterline testing methods are meant to detect and count elevated levels of representative heterotrophic species. These tests read a small sample from your waterlines and can provide an accurate count of colony forming units of planktonic heterotrophic bacteria within your waterlines - it should be noted, however, that "Bacteria counts can change rapidly, requiring repeated testing to reliably monitor water quality over time" (Dewhirst & Molinari, p. 13).
There are two primary differences with current testing methods to keep in mind. First, neutralization.
NEUTRALIZATION METHODS
If a waterline is being treated with a continuous low-level antimicrobial like a tablet, straw, cartridge, or drops, when samples are taken, the antimicrobial agent left in the lines will also be present within the sample. During incubation, whether through a mail-in laboratory test or in-office water test, the antimicrobial will continue to fight any bacteria present within the sample leading to false-negatives or more simply, inaccurate results.
If you test with a lab or in-office test that does not use validated neutralization methods for your treatment product, it is possible to pass a test when, in fact, the waterlines inside your practice are still above the ≤ 500 CFU/mL standard and unsafe for patient care.
So, to get accurate results, make sure the testing options you utilize include neutralization.
R2A VS MEMBRANE FILTRATION VS SIMPLATE METHODS
There are three current methods used in dental water laboratory testing: R2A, Membrane Filtration, and SimPlate. Understanding each of these will help you choose a laboratory sure to give you reliable accurate results.
Biofilm within dental waterline develop at room temperature - that is, around 20 degrees Celsius. At temperatures around 20 degrees Celsius, certain bacteria grow well, and others do not. Therefore, tests should be run at the same temperature to count the right organisms.
R2A and Membrane Filtration methods both incubate samples at this same temperature, allowing it to count bacteria most likely to grow within dental unit waterlines. Both of these methods are approved by OSAP in their white paper, "Dental Water Quality: Organization For Safety Asepsis and Prevention White Paper and Recommendations".
The SimPlate method was developed for non-dental purposes - to identify Escherichia coli (E-coli) - and incubates at 35 degrees Celsius, much warmer than room temperature. This allows it to best detect fast-growing organisms which can be very valuable in non-dental settings.
But with biofilm in dental unit waterlines growing at room temperature, this method misses too many organisms that could be residing in your dental unit waterlines.
R2A and SimPlate methods have been tested side by side by multiple universities for dental water testing and R2A has been set as the gold standard.
"When using a laboratory testing service, users should request that water be tested using the most current version of the spread plate R2A agar method (9215C) or membrane filtration method (9215D)..." - Organization for Safety, Asepsis and Prevention
Learn More About the Rationale for R2A Dental Water Testing Methods
HOW OFTEN SHOULD I TEST MY DENTAL WATERLINES?
Studies have shown that biofilm growth continues even 1-3 months after a treatment product is implemented in a practice's waterlines. Because of this, the OSAP suggests quarterly waterline testing. Some manufacturers and dental authorities have called for monthly testing.
The CDC, ADA, and OSAP reiterate that regular clinical monitoring of your waterline safety is the only way to ensure that treatment procedures are performed correctly and that your water exceeds the standard for safety (≤ 500 CFU/mL).
Follow these waterline testing frequency guidelines set by OSAP to ensure patient safety:
- Test within one month of implementing a treatment protocol - preferably, an effective one.
- Test your waterlines every month to start.
- Once you have all passing lines two months in a row, test quarterly.
Read OSAP's complete white paper and recommendations on dental water quality.
If a line fails during testing, initiate an immediate shock, confirm that maintenance procedures are being followed, and retest as soon as possible. If your test shows microbial counts in the caution range (200 to 500 CFU/mL), continue regular treatment, shock within one week and test at your next recommended interval.
HOW WILL TESTING MY DUWLS BENEFIT MY PRACTICE?
Each test product and laboratory are different; however, you can expect the following from all of them:
- All results will be measured against the CDC standard for safe water (≤ 500 CFU/mL)
- Samples will incubate for period of about one week
- You'll gain insight into the effectiveness of your treatment protocol
- You'll know whether your waterlines pose a risk to your patients and practice
- You'll have documentation showing your practice is following the CDC guidelines for safe waterlines
THE ONLY IN-OFFICE WATER TEST DESIGNED FOR DENTISTRY


Order Today!